A recent study shows people in Cardiff are struggling to get a good nights’ sleep with the city ranked worst for sleep problems.
People in Cardiff have seen their sleep suffer more than any other part of the UK during the lockdown according to the latest research.
Over 37% of people in the capital are suffering from insomnia according to research by Southampton University.
Professor Jane Falkingham, researcher of the report from the University of Southampton said, “We are seeing that Covid-19 is having a disproportionate impact on the health of individuals from different ethnic groups and those employed in certain jobs. The indirect impacts of Covid-19, including the closure of schools and businesses, and the move to home-working, seem to be worse for younger people and women. These factors may, in turn, impact upon sleep health.”
She said, “Disrupted and poor sleep is associated with wider mental and physical health challenges. Policy makers and health professionals need to take action now. It will be vital that they support and promote better sleep health.”
The ongoing COVID-19 crisis has made getting a good rest significantly harder.
“I’ve noticed sleeping issues since November 2019, but it started to affect my day to day life during the lockdown,” said an undergraduate student from Cardiff University adding that “it has definitely worsened over the pandemic.”
A poll conducted by the Royal Society for Public Health found out that two in five, which is almost 40% of employees reported a disturbance in their sleeping pattern over the pandemic.
The survey also highlighted that with the pandemic, more and more people are working from home and not getting a lot of exercises and natural light – both of which are important factors for a good nights’ sleep.
“I was sleeping all day and not seeing the light”
According to The Sleeping Council – a UK based organisation that aims to raise awareness of good nights’ sleep, depression and sleep disorders are closely linked. Insomnia is the most common and is estimated to occur in almost 75% of adult patients with depression.
Raj* A student from Cardiff University said, “My sleep cycle has been a mess for many years. This was caused by carelessness and also depression which caused me to isolate myself so I would stay up hours when everyone else was asleep.”
“For this week I have a prescription of Zopiclone to help induce sleep at earlier bedtime and to therefore fix my sleeping pattern,” he said.
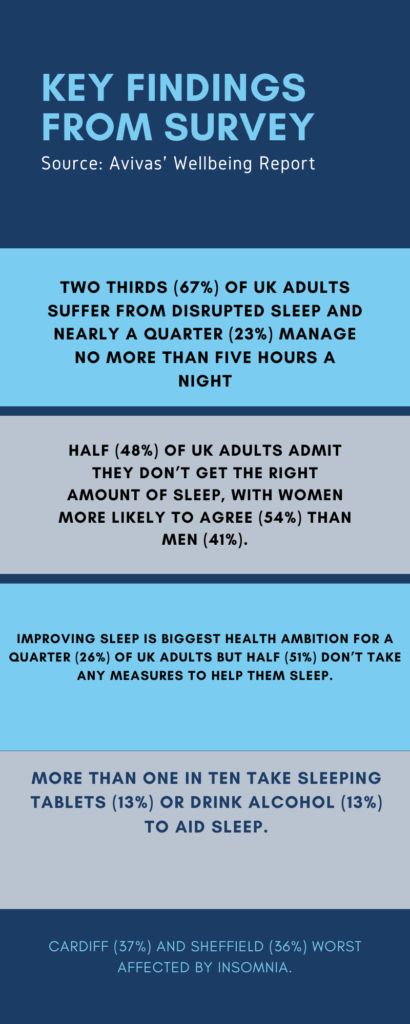
The study highlighted that sleeping peacefully is the biggest health ambition of people in the UK with 26% listing the same. More than half (51%) don’t currently take any measures to help them sleep better. Out of those who do, 13% depend on some kind of medication to help them sleep.
Chloe*, a 22-year-old Sociology undergraduate student at Cardiff University was diagnosed with insomnia at the age of 15. She has been prescribed sleeping tablets, however, she is only allowed to have 3-5 tablets in one prescription because doctors suspect she has bipolar type 2.
She said: “I don’t really understand why I am not allowed more than that, but I am usually given Zopiclone. Sometimes I can’t sleep for two days and start to have auditory hallucinations. I have periods where I’m totally unaffected by it and I am able to sleep.”
“I usually tend to be high energy but low mood when I’m sad so I struggle to sleep when I have things going on my mind feels like 100mph but sometimes my brain is like not there and I just feel very absent and will sleep 15+ hours,” she said.
According to the NHS website, Zopiclone is usually provided to patients to treat insomnia. The website also highlights that patients can become dependent on it very quickly.
Dr Simon Braybrook of Butetown Medical said, “It’s like a withdrawal from heroin. I think it’s one of the worst withdrawals you can have.”
Another student from Cardiff University suffering from insomnia opted for herbal sleeping pills instead of prescription medication, reporting that they “helped a little as it reduced anxiety and let me sleep but if I’m more anxious it doesn’t work.”
Sleep deprivation is also linked to reduced productivity. A study into the economical effect of sleep deprivation highlighted that poor quality of sleep amongst UK workers was losing the country 1.86% of its GDP. According to the researchers, if people who sleep under six hours began sleeping to seven hours, this could add £24.5bn to the economy.
Afreen*, a 32-year-old postgraduate student reported that she felt “Extremely distracted like I would experience depersonalization all day long.” Further, she said: “With time I have gotten used to it and schedule my work around it when I feel more alert and awake and sleep when I’m sleepy or tired.”
A study provides evidence that insomnia may cause dysfunction in emotional difficulty as well as the development of depression and other problems.
She said, “It is emotionally and mentally it is challenging because it also causes a lot of brain fog making it difficult to think clearly and cannot process things efficiently and days go by in a daze. Not sleeping properly messed with circadian rhythm and eventually appetite.” However, she has been able to improve the quality of her sleep cycle by “intermittent fasting, balancing food portions and strengthening exercises throughout the day.”
The report also highlighted that 13% of those surveyed resort to alcohol as a ‘night cap’ to help them sleep better.
A study by Alcohol Rehab highlighted that alcohol dependency and insomnia commonly co-exist as many who can’t sleep turn to alcohol in order to get rest.
Matt, a 23-year-old student from Cardiff University says he doesn’t remember the last time he was able to sleep peacefully “Without alcohol being involved.”
He said, “It helps mentally to drink before trying to sleep as it stops me from dwelling so much on past events or worrying about the future but it takes a mental toll knowing that I maybe becoming dependent on alcohol to sleep properly.”
Dr Doug Wright, Medical Director at Aviva UK Health, said: “Alcohol can also lead to disrupted sleep and a ‘night cap’ to aid sleep can actually have the opposite effect.
“There are lots of methods available to help aid sleep, such as avoiding devices close to bedtime, controlling light and noise levels.”
Afreen said, “I do try to follow a routine but it’s hard to stick to depending on my mood. Things I usually do are I have a hot bath before bed, I apply some castor oil on my eyes and forehead (i feel it helps), I keep my room cool and wear lightweight clothes, my duvet is heavy so that helps with the restlessness, I also keep a small fan to provide constant white noise.”

*Names have changed at request to keep identities confidential and anonymous


