But there’s ‘room for improvement’ in the number of 12 to 13-year-olds having the HPV jab
The number of children in Wales who are taking the HPV vaccine, which targets the types of virus that commonly cause cervical cancer, has increased after numbers fell during the Covid pandemic.
The uptake of the jab, which is given to children aged 12-13 in two doses, is now at 83.2% for the first dose and 72% for the second. That’s an increase from 55% for both doses in 2021. HPV, which stands for Human Papillomavirus, is a common virus that can, in rare cases, develop into cervical cancer if left undetected.
Dr Chris Johnson, head of the vaccine preventable disease programme for Public Health Wales, said that there is “room for improvement” to encourage more children to have the vaccine.
He said: “In Wales, uptake of the crucial first dose of the HPV vaccine by school year 10 in 2021-22 is high at 83.1%, and is at 72.7% for the second dose.
“This is because of significant efforts by our vaccination teams, after uptake in this age group was affected during the Covid pandemic.
“However, we recognise that there is room for improvement, and we will be working with partners to do more to promote the vaccination and encourage take up across Wales.
“The World Health Organisation strategy for the elimination of cervical cancer sets out that to achieve elimination of cervical cancer in girls with HPV, vaccination should be at 90 per cent by the age of 15.”
Cervical cancer charity Jo’s Trust launches its annual Cervical Cancer Prevention Week (January 23-29) to raise awareness of cervical cancer and to drive uptake in the NHS Cervical Screening Programme.
853 women in the UK died from cervical cancer between 2017-2019, with 52 of those from Wales. Yet it is the most preventable cancer. There are about 160 cases of cervical cancer diagnosed every year in Wales and it is the second most common cancer amongst women under 35.
Although Jo’s Trust runs a Cervical Cancer Prevention Week every year, in 2023 the trust is launching its “biggest ever campaign.” This year, the End Cervical Cancer campaign is focused on eliminating the cancer by “tackling inequalities in cervical cancer prevention, ensuring we have the technology and workforces we need, and researching better and more effective ways to prevent cancer”.
The charity is calling for the UK government to demonstrate a commitment and create clear strategies to eliminate cervical cancer – such as the World Health Organisation’s strategy.
Jenny Rathbone, who is a Member of the Senedd, has been campaigning for cervical cancer awareness for more than two decades.

“This is a very important matter that I take great interest in,” said Ms Rathbone, pictured left. “I spent a lot of time in the 1990s making sure that GPs were complying with ensuring that all their female patients were getting tested where possible.
“The test is now much more sophisticated than it used to be, so we can see well in advance where there may be cells that are starting to display signs of HPV development. That’s why we can comfortably see women in less than five year intervals.
“Science has moved on a lot in this field, for what has been historically a very difficult cancer to identify early on and therefore treat – by the time anyone would realise what’s happening, it’s spread elsewhere.”
And she had this advice for women: “Make sure you or your daughter takes up the HPV vaccine, and if you haven’t had the cervical smear test yet, make sure you go and get one.”
What is Cervical Cancer?
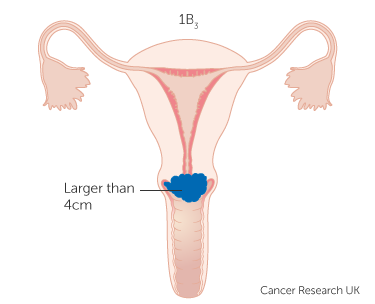
Cervical cancer is cancer affecting the cervix. This is the entrance to the womb, located inside the vagina. Almost all cervical cancer cases (99.8%) are caused by a virus called human papillomavirus, or HPV.
In most people, HPV does not cause any problems and the body will get rid of the virus on its own. HPV is spread by skin to skin contact, and is transmitted into the cervix by sexual contact.
High-risk types of HPV can cause changes in the cells of the skin covering cervix, called cervical intraepithelial neoplasia (CIN). Most CIN will go away on its own, but sometimes it can get worse and develop into cervical cancer (as pictured).
What is HPV vaccination?
From September 2019, everyone in Wales aged 12-13 was offered the HPV vaccination. The vaccine covers the most common (high-risk) types of the virus, which cause around 70% of cervical cancers. Some cervical cancers are caused by different HPV types, which the vaccine does not cover. Therefore, people who have been vaccinated should still have their cervical screening tests when invited to do so.
The vaccine is given to girls and boys aged 12-13 because it should be given before they might come into contact with HPV.
What is a smear test?
Cervical screening, or a smear test, is when a small sample of cells is taken from the cervix and tested for the presence of HPV.
The test itself usually takes less than five minutes, making the whole appointment around 10 minutes long, and is usually carried out by a female nurse or doctor.
If high-risk HPV are not found, you do not need any further tests. If these types of HPV are found, the sample is then checked for any changes in the cells of your cervix. These can then be treated before they get a chance to turn into cervical cancer.
The HPV virus can lie dormant for many years and may never cause any cell changes.The virus might cause cell changes many years later, having been in the cervix for years with no issue. This is why it is important to keep going for screening when you are invited, even if your tests have always been normal.
Many of the symptoms caused by cell changes are similar to other conditions. This is why cervical screening is important.
Who is eligible for screening?
The UK National Screening Committee has recommended that cervical screening programmes invite all people with a cervix, aged between 25 and 64 every five years once they have tested negative for HPV.
Cervical Screening Wales (CSW) is only able to invite individuals who are registered with their GP as female, or indeterminate/unspecified. If you are registered as male, but have a cervix, you can still have cervical screening by contacting your GP.
In 2018, Cervical Screening Wales introduced screening using HPV testing. This test is more effective at identifying people at higher risk of developing cell changes which can cause cervical cancer.
If no high-risk HPV is found in a woman’s sample, the risk of developing cervical cancer within the next five years is very low, as it takes around 15-20 years to develop after infection with HPV.
Due to this research, Cervical Screening Wales changed the waiting time for cervical screening from three years to five years in January 2022. The change was implemented in Scotland in March 2020 and will be adopted by England in the future.
Why aren’t people attending screening?
In Cardiff and Vale, the number of women screened for cervical cancer was 71.6%, with the national number of women screened at 73.2%. Previous estimates suggest screening prevents 70% of cervical cancer deaths, but 83% of deaths could be prevented if everyone attended regularly
As part of the Help Us Help You campaign in 2022, a survey of 3,000 women and people with a cervix commissioned by DHSC reveals a number of concerns which prevent cervical screening.
Embarrassment was the most common reason for never having attended or missing an appointment (stated by 42% of respondents), followed by those who “kept putting it off” (34%) and “being worried it would be painful” (28%). Fifteen per cent of lesbian or bisexual women over 25 had never had a smear test, compared with 7% of women over 25 in general.
Public Health Wales has offered advice to anyone who’s nervous about getting a smear test:
A spokesperson said: “It’s natural to feel nervous about your screening. But don’t let that discourage you from putting it off or avoiding the appointment altogether. The screening process is ultimately a safe way to prevent cervical cancer from developing. And although it might feel uncomfortable for a few short seconds—it’s worth it in the long run. If you’re feeling nervous about your screening, these calming techniques can help:
• Focus on your in-breath and your out-breath.
• Focus on five things you can see, four things you can hear, three things you can feel, two things you can smell and one thing you can taste.
• Relax your body bit by bit. Focus on relaxing the muscles in your face, arms, legs and back.
• Listen to music.”
If you are concerned about your symptoms or want to arrange a cervical screening, contact your GP or Cervical Screening Wales.