As long waiting lists for glaucoma patients pose a severe threat to their eyesight, a new initiative in Cardiff aims to provide training to optometrists and shorten waiting times.

A new initiative in Cardiff aims to tackle the waiting list backlog for an eye disease that affects thousands of people in Wales.
By training more optometrists, the NHS Wales University Eye Care Centre targets the backlog of glaucoma patients.
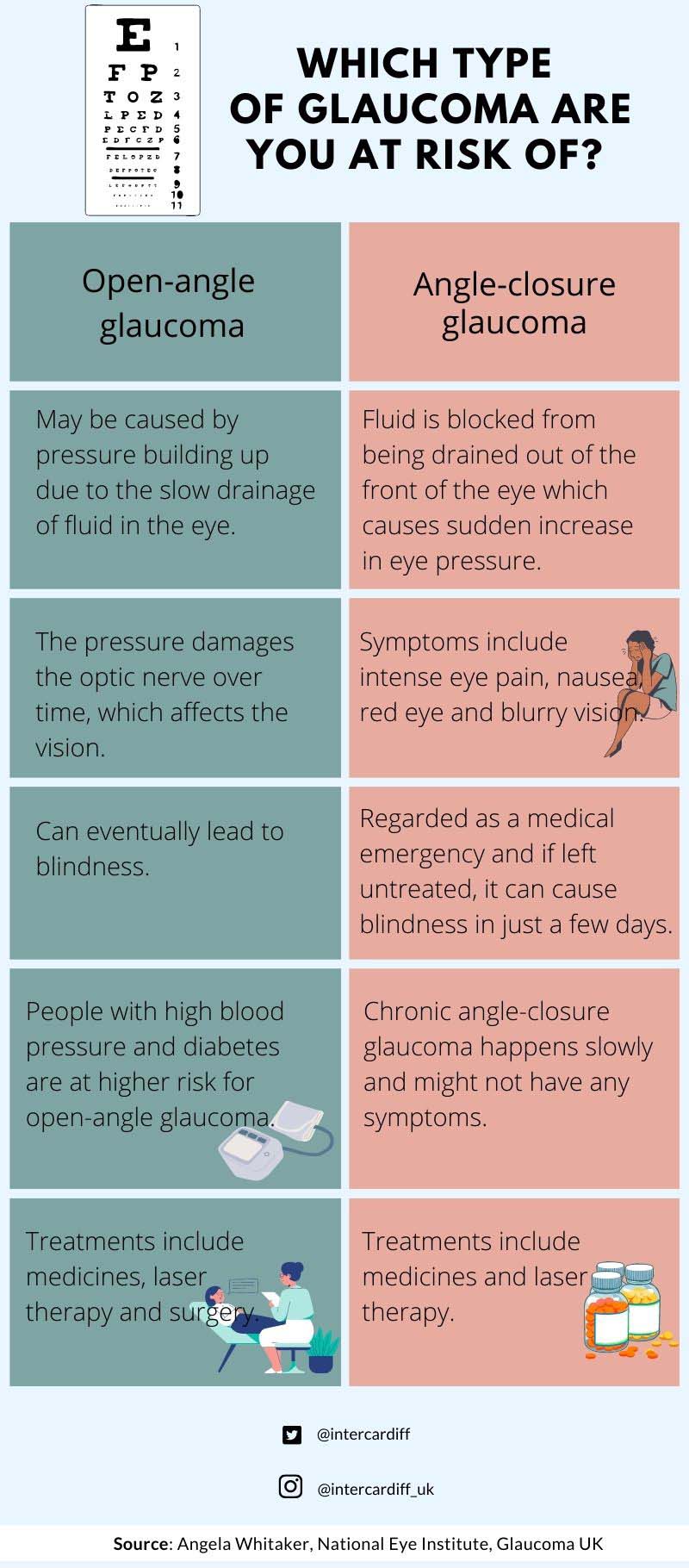
Glaucoma is a disease that causes nerve damage in the eye, and it becomes increasingly risky with age. It is a difficult illness to detect, and waiting times are particularly high because of the level of treatment each patient needs.
“It can only be detected when they go for a routine sight test at a community optometry practice; that’s usually where they get detected,” said Angela Whitaker, senior lecturer at Cardiff University School of Optometry. “They don’t notice that they’re getting blind spots in their vision and in their visual field until it’s too late. And once they’ve got that damage, you can’t get it back.”

“It’s not like an operation for a cataract where you go in, you have an operation, you get discharged and that’s it. For glaucoma, you need to have regular checks, depending on your condition every six months or nine months or 12 months for the rest of your life. So we keep gaining patients and the numbers just go up and up and up,” said Angela.
The clinic, which sees around 24 patients per week, was set up by Cardiff University in collaboration with Cardiff and Vale University Health Board to tackle the backlog of delayed glaucoma appointments in September 2021. This was an issue that the NHS has been facing for a while, which was further worsened during the pandemic.
“The patient feedback has been absolutely outstanding. They don’t have to wait two hours to see the doctor. Almost all of them say that they’d like their next appointment to come back to us,” said Angela.
Unfortunately, the most common type of glaucoma in the UK does not have noticeable symptoms, according to Angela, who is also the clinical lead.
A major risk factor to glaucoma is raised pressure in the eye. Although there is no visible damage to the eye that a patient would notice themselves, it must be treated to prevent loss of vision, according to Angela.
Angela said that the main reason for the appointment delays was because of lack of capacity and struggles to keep up with the demand for appointments as glaucoma patients need regular checkups.
“At the moment, the only way to prevent or delay the start of glaucoma is by treating eye pressure in susceptible individuals. Those people would normally be picked up by community optometrists and referred to the NHS to see if they need treatment to reduce their risk of developing glaucoma, so therefore, they form part of our workload as well,” she said.
There have been incidents that were reported nationally, where patients who’ve had delays to their appointments for months and even for over a year, have lost their sight.
A glaucoma patient in Cardiff who decided against enrolling in the NHS waitlist because of the long waiting time, said, “I’m getting treated privately. It’s very expensive and if not for insurance, I do not know how I would be able to afford the treatment. We definitely need initiatives like this which will help people get treatment and assessment of their problem in a timely manner.”

Until about 20 years ago, patients diagnosed with glaucoma were assessed and treated by ophthalmologists who were specialists in glaucoma, according to Angela. Now, the professional landscape has changed, as the demand for treatment services has grown, and non-medical eye practitioners such as optometrists treat more patients.
“So, one of the main ways to improve capacity in the system and thus reduce the waiting times for patients is to use other staff because there’s always a shortage of doctors. But there isn’t a shortage of optometrists. So, we can step up and train, and actually so can other eye care practitioners such as nursing colleagues and orthoptists as well,” said Angela.
Eluned Morgan, Minister for Health and Social Services said, “Ophthalmology services has seen a significant increase in demand over recent years and we don’t want people to risk their sight by having to wait a long time for treatment. Improving access to treatment is vital if we want to cut waiting times and ensure eye care services are fit for the future.”
Angela noted that some challenges to setting up the clinic included getting the equipment, digitising the medical records, as well as providing glaucoma training to optometrists.
Angela believes that expanding training opportunities can guide optometrists and in turn, people who are at the risk of visual impairment can benefit from early diagnosis and receive prompt treatment.