Two-thirds of hearing impaired people in the UK do not have an accessible way of contacting their GP. Just how much of a challenge do they face in Cardiff?

As Jenny lay in the hospital room sedated, she couldn’t hear anything. She did not have her hearing aids, and there was no one to take her home. The face masks made it harder for her to lip-read what the doctors were asking her.
She was helpless and terrified, even though she had nothing to be worried about. Her hearing loss had made a regular surgery so much more painful, and she had to wait for days until she received written documents assuring her that her procedure had been successful.
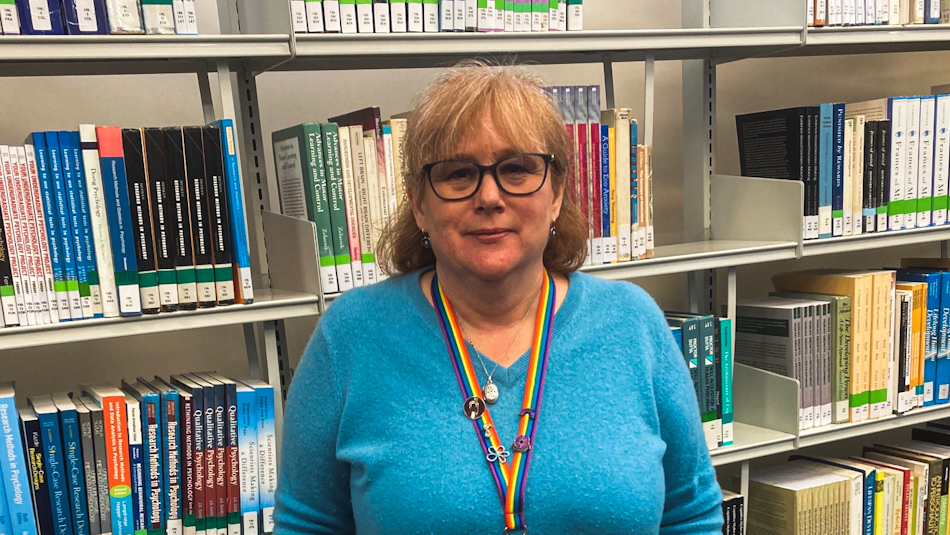
Jenny’s hospital experience was one of the many challenges in her life as a deaf person. “I know what it was like to have my independence before,” she says. “For somebody who’s always been able to do things on my own to now having to rely on someone to help you understand something that’s going on… it can be very frustrating. Any confidentiality you might have goes through the window.”
She has bilateral hearing loss, making her deaf in both ears. She lost her hearing gradually, a result of “too many loud rock concerts” in her teenage years, she believes.
Booking appointments with the general practitioner (GP) has always spelt trouble for her as she would have to rely on her husband to listen to the telephone conversations and tell her what is going on.
Jenny is not alone in this struggle. According to a recent report by a group of charities in England, 67 per cent of deaf people do not have an accessible way of contacting their GP. There were demands made to the NHS by the charities to improve communication with healthcare providers on medical information and provide cost-friendly services.
Another report by All Wales Deaf Mental Health and Wellbeing Group reveals that deaf people still do not receive information in ways that they can understand and engage with. A major knowledge gap persists as healthcare specialists are unaware of counselling services for them. The closest place for treatment where medical professionals can fully communicate in British Sign Language (BSL) is London, Birmingham or Manchester.
Naomi Wray, President of the BSL Society at Cardiff University, is fully deaf and a wearer of cochlear implants — electronic devices that help her hear. She found it incredibly difficult to communicate with her GP, who would rush through the process of asking questions, which she could hardly understand.

“Any time I asked him to repeat it, it was like I was a massive inconvenience to him,” she says. “It’s just completely put me off having a GP in Cardiff, which I think is incredibly unsafe and unhealthy,” she says. “I don’t want to agree to anything when I don’t properly know the details. This is to do with my health. These are important questions. I need to hear them.”
The entire process was tiring and overly complicated for Naomi. She had to go to a pharmacist to be able to speak to them face-to-face and get advice. She eventually transferred to a GP back home in Hertfordshire, with whom she now communicates via email.
Like Naomi, Jenny has also faced difficulties with her GP. The process of contacting a GP is via telephones, which is not possible for deaf people without hearing aids. Jenny has accepted the fact that “they’ve got issues”. Although she managed to get a face-to-face appointment with her doctor last spring, she agrees that not everyone can get that opportunity and that healthcare professionals need to resort to alternate means of communication.
“There are technologies that are free like Zoom… you could do your appointment via a video link, which would make it easier for a lot of people,” she says. “Because at least you can have captioning or lip reading.”
Moving forward, Jenny believes that if healthcare services become more aware of deafness and how to deal with deaf people, we might see a positive change. “We’re going to see more online and less face-to-face appointments for certain things,” says Jenny. “And if that’s the case, they need to use and embrace the technologies that are out there to enable people like me to access them fully.”
For help and support, contact RNID by sending them a text message on 07360 268 988.

