This week marks the end of Endometriosis Action Month. InterCardiff talks to some women who suffer from this disease to learn about their experience.

As Alex rolled over in bed, a sudden pain caused her to curl into a tight ball under the duvet. Daylight was streaming through the curtains, and it was time for her to get up for work, but the pain wouldn’t let her. She had to call in sick.
Alex has been struggling with endometriosis for many years, and has striven to make people who don’t understand the condition aware of the pain endured by patients. On Sunday, she and others came together to march through Cardiff’s city center. “We are one in ten! We need a diagnosis now!”Everyone shouted in unison.
Alex Hazlehurst, 40, one of the organizers of the march, said: “It took twelve years for me to get a diagnosis. I’ve had to fight to get access to treatment ever since. Our most common difficulty seems to be getting doctors to take them seriously. The average wait for a diagnosis in Wales is ten years, and that’s just not acceptable.”
March is Endometriosis Action Month in the UK, and this year’s theme is “Endometriosis Explained.” Worldwide EndoMarch, the organizer of this march collaborated with Fair Treatment for Women Wales(FTWW). Women in Cardiff who suffer from the disease have also taken to the streets to shout their inner thoughts in a commitment to raise awareness of endometriosis.
Alex has had 11 operations in 15 years, which have severely affected her work. She had a hysterectomy at the age of 38, and the physical toll of such a treatment regimen on a woman is undoubtedly enormous.
This experience is echoed by many. Donna Baldwin, a march participant, 42, recalled the years of being overlooked by doctors. “I started having symptoms when I was around eleven. I went back and forth to doctors, but I was ignored and told it was all in my head or that it was normal. It actually took me 23 years to get diagnosed. I finally got referred to an endometriosis team when I was having fertility issues.”

Similarly to Alex, she had a hysterectomy about a year ago. The long wait for a diagnosis changed her entire life: “I can’t function as a person anymore. I used to be an actor, but I can’t tour or do shows anymore. I don’t know how I’ll be able to hold down a full-time job again. I struggle to visit family who live about three hours away.”
Donna also mentioned the pain of not being understood: “People say, ‘Oh, you’ve had surgery, you’ve had a diagnosis, you should be okay now.’ But this isn’t a condition that can just be fixed or treated. When you meet someone living with chronic pain, they might seem okay. Right now, I’m talking to you, I’m not wincing or crying, but my body is in pain from head to toe. We’re very good at masking it. It would be nice if people would accept that this is actually a disability and show more care and understanding.”
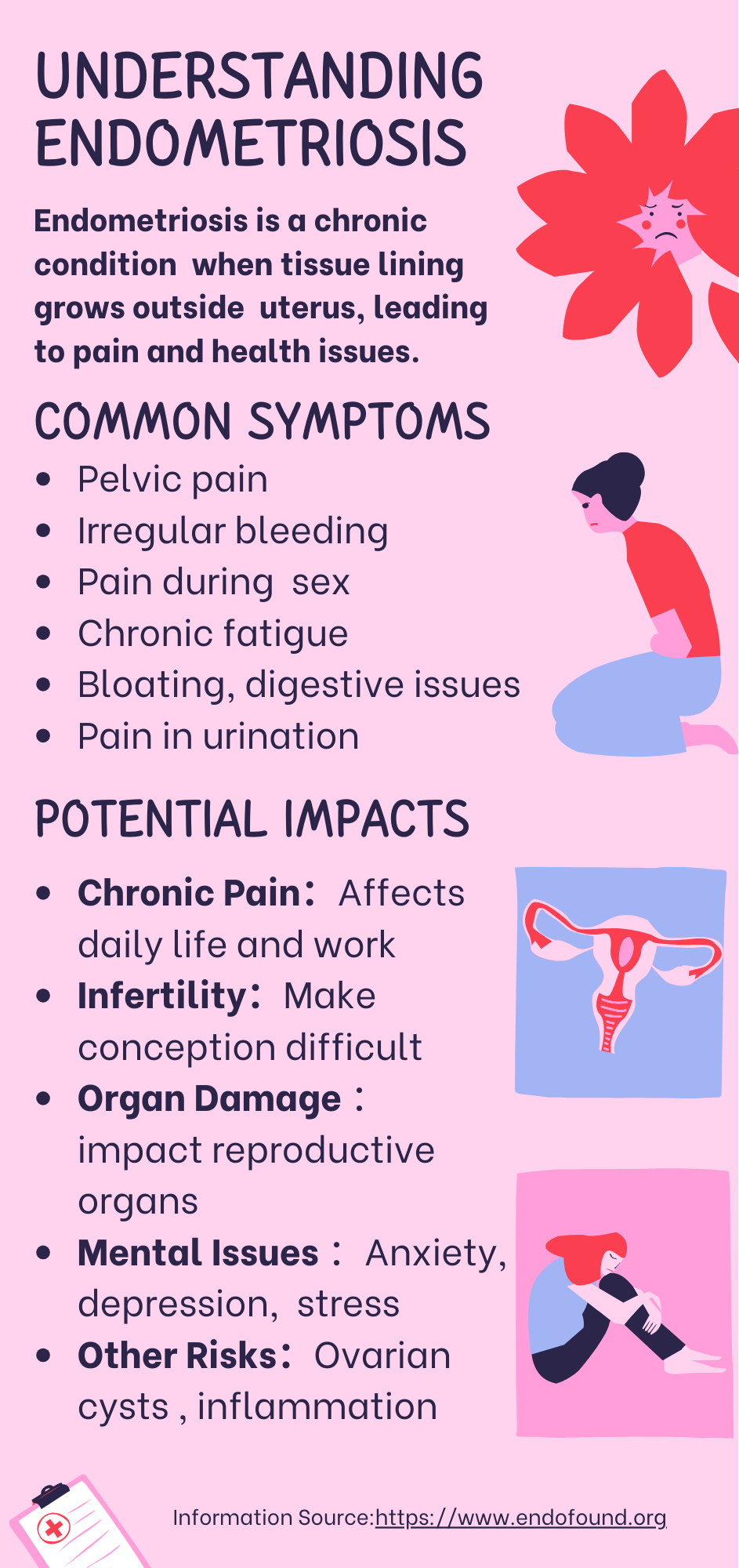
Endometriosis impacts one in ten women in the UK. It is far more than just a painful period. In severe cases, the condition can lead to organ damage, fertility issues, and long-term complications. Yet, many sufferers are dismissed, prescribed painkillers, or advised to undergo invasive surgeries without fully understanding their options.

Participant Zoe Hughes said the only reason she got diagnosed was because she paid to go private: “Most of the doctors I saw were male, I was told it was normal, that periods are supposed to hurt. There’s a lack of medical professionals who have proper knowledge about endometriosis. Even the good doctors have given me incorrect information. The only real support I’ve found is from other people who have the condition and share their experiences.”
The struggle doesn’t end with a diagnosis. There is still a lot of support needed for women with the disease. Donna said: “Once you’re diagnosed, you’re then thrown into another battle with the system to get referrals for things like physiotherapy.
“Even when you do get the referrals, you might end up with someone who doesn’t understand endometriosis and can’t provide the right treatment. I don’t want to just rely on painkillers and medication. I want to explore as many alternative treatment options as possible, but getting those referrals is nearly impossible. The waiting lists are unbelievably long.”

There are currently only two endometriosis specialists in Wales, and the University Hospital of Wales in Cardiff is the only specialist centre. In March 2022, the Welsh Government appointed dedicated endometriosis nurses to every health board in Walesin order to improve the situation.
Alex said there is still room for further effort: “There needs to be far more awareness, and we need to get endometriosis recognized as a whole-body disease, not just a gynecological disease. Endometriosis has been found in every organ of the body. We need to train more specialists from different disciplines in medicine. That way, women will have better access to treatment. That needs to change very quickly.”