In occasion of the upcoming International Nurses Day let’s reflect if it is time to start truly reevaluating their role. Here, some stories of how the pandemic has affected these essential workers.

It was not the first time James had cared for a Covid-19 patient in the intensive care unit, but it was the time that brought him closest to a collapse. He was indicated with a patient who had a tracheotomy. The patient’s head was tilted back slightly, towards the ceiling above. Several instruments flickered aside to maintain his feeble breathing.
“The ventilator was disconnected from the trachea and the secretions came out, flying out, into my face shield, my neck, and my gown. At that moment I had a panic attack. I felt that I was compromised and contaminated,” he said, dropping his eyes.
James Frank has been an intensive care unit staff nurse at a hospital in north Wales since the autumn of 2014. At the early stages of the Covid-19 pandemic, the biggest challenge for him and many of his colleagues was how to provide efficient critical care whilst protecting themselves with the available equipment.
Personal protective equipment, a solid line of defense on the frontline against the Covid-19, was feared by medical staff to be in serious short supply during the first wave. Furthermore, even with the protection of the PPE, they are not completely safe.
Caroline Evans, a private nurse at Richmond Nursing Agency in Llanelli, is among the many nurses who had the misfortune to be infected.
Before the outbreak of Covid-19, Caroline has started her part time business in different therapies while working as an agency nurse. Then things changed direction. “I had to stop my therapies and work full time on the covid patients,” she said, feeling the strain and stress coming back.
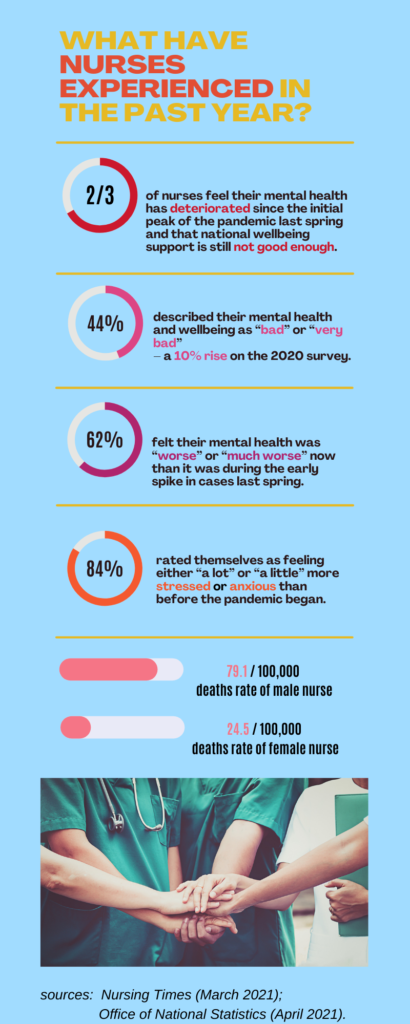
While citizens were clapping, nurses were facing fear of contamination, work burnout, mental challenges as well as social stigma. “I became very emotional and drained although I wanted to help others during the difficult time,” said Caroline.
James had a deeper feeling: “People think that we have the virus ourselves just because we are taking care of the patients who have been infected.” This, together with the fear of uncertainty and the high intensity of work have taken a heavy toll on him. He described the situation as “physically, mentally, spiritually exhausting”.
“We were very anxious about this pandemic,” he recalls the experience when he was indicated with a patient who had a tracheotomy. He soon got a prophylactic treatment after being splashed with the secretion. But he was still afraid because he had to go home. “I was like, well, I have been compromised now and, should I go home now? Because my family will likely be compromised as well.

(© International Council of Nurses)
The experience and fear of being infected is not the most upsetting thing for them.
“The hardest thing for me was when some patients passed away with no family presence. I was grateful to hold their hands. But it’s really hard to see them pass away taking the last breath and not being able to have anyone there,” he said.
For Caroline, “the hardest thing was looking after people who were ill with a virus that I wasn’t familiar with. I felt helpless and not confident. I tried my best; things didn’t really seem changed for me.”
After witnessing the passing of life up close, they still had difficulty facing this cruel thing.
The lockdown from Christmas to spring and the vaccinations coverage have taken the pressure off many nurses. Although sometimes James and his colleagues are still uncertain with “where we are going with the pandemic and the psychological trauma that crops up”, he is still “hopeful and confident that things are getting better now”.
As a result of this extreme situation, the theme of this year International Nurses Day celebrated on May 12 is A voice to Lead, A Vision for Future Healthcare. This indeed aims to rethink the profession and seeking innovations to enter into the next stage of healthcare, while coping with the unprecedented global health crisis.
Talking about the future, James said: “The nursing profession, as I think, is the combination of healing science and art that bands us all together as human beings who love and care for all. We must continue to strengthen our professional training, especially for disaster prevention, responding and recovery.”
“I hope to leave nursing in the future to become a full-time therapist,” Caroline said, explaining that the experience of the epidemic has strengthened her belief. She said: “I need to do what I really want to do once all this is over, the therapies that help others with their anxieties and stresses.
“We should now be able to consider the wellbeing of nurses and change things for the better. Nurses should be respected and feel proud in the future to maintain its professionalism.”